The best way to think about what might cause one’s breasts to descend on the chest over time is to consider that the breast has an external ‘envelope’ of skin, and internal volume of soft tissue made of fat and glandular tissue. When the internal breast tissue volume no longer fills the skin envelope, a deflated appearance develops. Conversely, if the skin stretches around the inner soft tissue, again a deflated appearance can develop. Women may choose to undergo mastopexy surgery to address:
- Stretched breast skin, often following breast feeding or pregnancy.
- Stretched breast skin remaining as a result of significant weight loss.
- The natural effect of aging on breast tissue.
- Asymmetric breasts, where one sits naturally lower than the other.
Depending on the balance between internal breast tissue volume and the skin envelope, Richard may recommend the placement of a breast implant as well as redraping and tightening of the breast skin. This is called an ‘augmentation-mastopexy’.
What can I expect?
A mastopexy can elevate the position of the breast and tighten the breast skin, creating a more projected and perky shape. The nipple is raised up on the chest, whilst the underlying glandular tissue repositioned and shaped. To do this, Richard needs to remove that excess skin, redraping the breast tissue. Despite this highly effective technique, the breast shape will still continue to be affected by changes in body weight, skin stretch, ageing, pregnancy and of course, gravity. As such, it’s really important to approach a mastopexy with a stable body weight.
What happens before surgery?
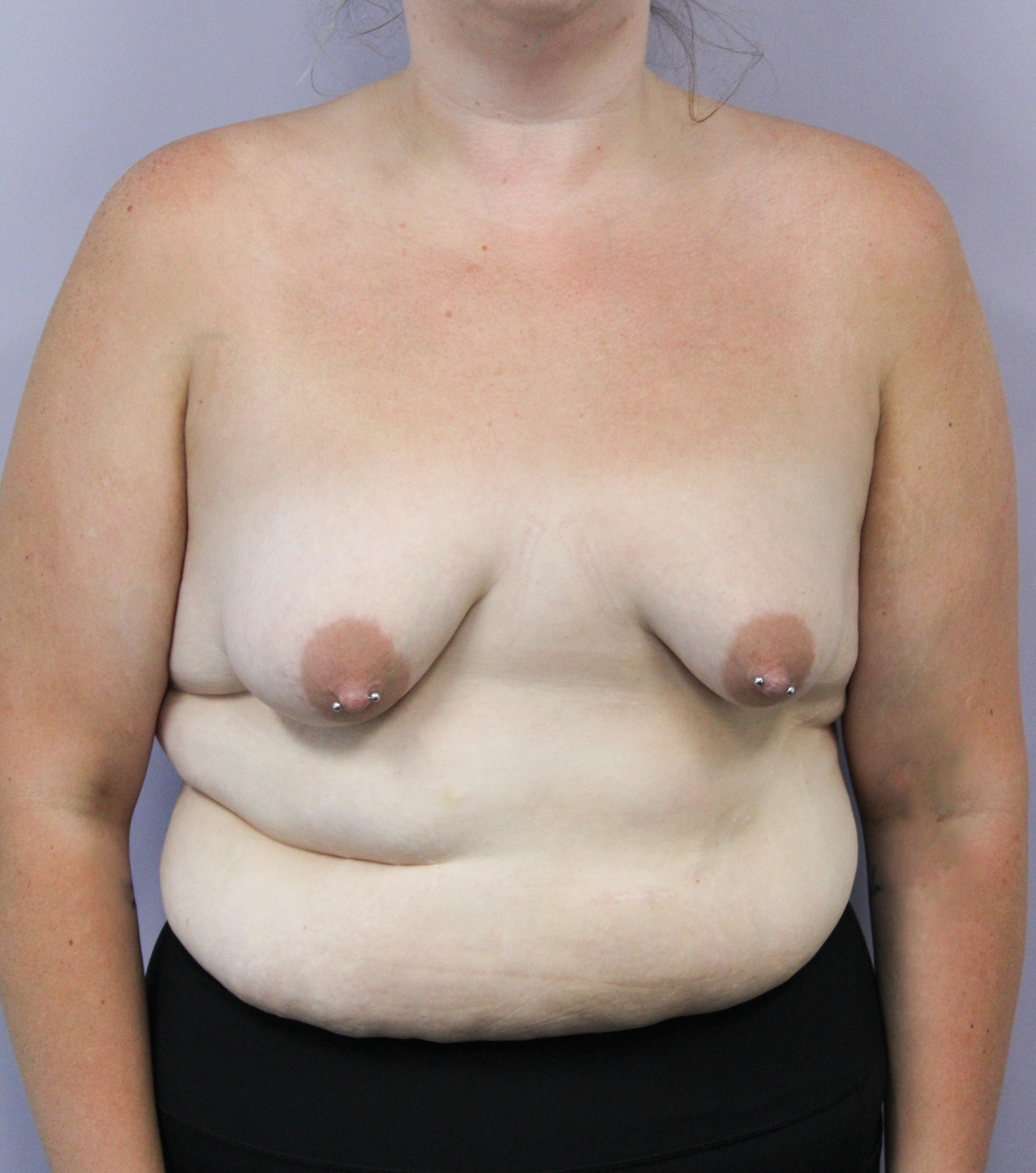
As part of your consultations, you will be able to describe your desired breast shape, and together with Richard, you can make some decisions about how best to achieve this. Richard will make some routine measurements to help plan your surgery and take pre-operative photographs. As with all surgeries, Richard will need to know about your body weight, height, other medical issues and smoking status.
What happens during surgery?
On the day of surgery, you’ll arrive in the hospital, paperwork checked and taken up to theatre. You’ll have a chance to speak with your Anaesthetist and Richard prior to surgery, and Richard will make some surgical markings on your breasts to help guide during surgery. In theatre, your Anaesthetist will place you safely under general anaesthetic, monitoring your health throughout the procedure. Richard will meticulously undertake your surgery and ensure the final shape. Richard doesn’t routinely use surgical drains. A surgical bra will be placed over your light dressings whilst you’re still asleep, then you will be taken out to the recovery room where you will wake up.
What happens after surgery?
Most patients go home the same day or the day after surgery, and you should plan to have an adult around to help for the first few days or so you can concentrate on your recovery. You should expect a moderate degree of discomfort, which settles over the first week or two. This is most often controlled by regular oral analgesia as guided by your Anaesthetist. It’s really important to keep your surgical bra on full time for the first month, and no upper body weights or heavy lifting for a month and 6 weeks before jogging. You’ll be seen in our rooms at one week to ensure you’re doing well and at around six weeks with Richard. As always, please don’t hesitate to contact us if you have any concerns. Over the coming 6-12 months, your shape will settle and scars start to mature.
Possible complications:
The decision to undergo mastopexy surgery should only be made after considering if the potential benefits can achieve your aims, and whether the risks are acceptable to you. The possible risks/ complications of mastopexy include (but are not limited to):
- Cardiac problems, including heart attack or arrythmias.
- Venous thromboembolism (including deep vein thrombosis and pulmonary embolism, which may be fatal).
- Surgical site infection, including of any implants (if used) which may necessitate removal of that implant.
- Haematoma requiring return to theatre.
- Wound breakdown, delayed healing or protruding sutures.
- Nipple/ areolar necrosis (partial/ total).
- Conspicuous scars, including hypertrophic, stretched or migrated scars.
- Altered sensation to the breast, nipple or areola. This may be increased (hypersensitivity) or reduced sensation. This may be permanent or temporary.
- Possible need for revisional surgery. Richard will only consider revising your breast augmentation if he believes:
- there is a definable structural issue with your breast,
- this issue is realistically able to be improved with surgery and
- the risk of revisional surgery causing a worse result are minimal.
- Dissatisfaction with the degree of breast lift.
- Breast asymmetry or non-round areolae
- Resorption or failure of fat grafting (if undertaken).
- In the case where an implant is also inserted as part of an augmentation-mastopexy procedure, the same risks exist as per both breast implant augmentation and mastopexy. Further, some of these risks may be more likely, such as wound breakdown or skin necrosis (where some breast skin doesn’t survive).